This is Part 1 in our series on preparing to return to ‘normal’ operations after COVID-19. Read the introduction here, Part 2 here and Part 3 here.
Background and Framework
On March 18, Vice President Pence asked that all health systems delay elective surgeries and focus operations on preparing for the potential influx of COVID-19 patients. The vast majority of hospitals complied with this request and 35 states expressly forbid the continuation of elective surgeries.
Given this backdrop, many hospitals and health systems are now facing various levels of pent-up demand for both postponed and future surgeries, while also balancing limited resources, capacity constraints, and ongoing COVID-19 quality and safety concerns. These topics are manifesting themselves in questions such as:
- Given limited resources, how should we prioritize patients? Do we triage by medical necessity, ensure even access across service lines, or even prioritize marquis cases to help relieve financial pressures?
- How many patients and cases were cancelled or will be cancelled in the near future? Are there cases that will never return? Are there opportunities for us to treat cases that other hospitals in our market are not prepared to treat?
- Are there ways to expand our capacity, such as extending OR hours? Will our already stretched clinical teams be available to cover weekend and evening operations?
Answers to these questions lead to even more questions, ultimately resulting in a relentless cycle of questions, data and analysis that can paralyze any management team. At KCG, we have encouraged our clients to establish a governance team charged to link and coordinate resources across the organization to facilitate the re-opening process. These multi-disciplinary teams span the health system’s operations and leverage subject matter experts [SMEs] as necessary; however, these teams should also be nimble enough to enact change without placating every stakeholder. Through cooperative efforts with these teams, KCG has developed a framework that empowers them to analyze the data and collaboratively create their re-opening plan. The framework consists of three specific focus areas, as depicted below:
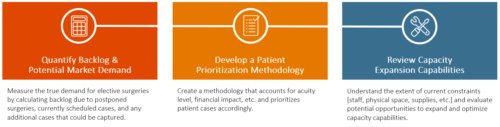
Each of these focus areas will be explored in greater detail in the following sections of this post as we pose actions and questions each health system should consider as they seek to develop their own re-opening plan.
Approach and Work Activities
Quantify Backlog & Potential Market Demand
At a minimum, nearly 6 weeks of elective procedures have been cancelled or delayed – and for those regions most impacted by COVID-19, this number may be much higher. In addition, each hospital has previously scheduled appointments that may extend months into the future. Lastly, there may be opportunities to acquire new patients from competitor systems that are struggling to reboot their operations.
The first step in returning to normal is to quantify these three distinct patient groups and identify the ‘true’ demand. While not an exhaustive list, here are a few questions that some of our health system clients are considering:
- What did our volume look like 12 months ago and what could it look like in three, six, nine months from now?
- Utilize market and/or claims data to compare pre-pandemic volumes to current volumes and overlay on anticipated future volumes.
- Review projections released by the Institute for Health Metrics and Evaluation [IHME] and others; establish a list of probable scenarios our system should plan for [prolonged outbreak, second wave, etc.]
- Develop a modeling tool capable of evaluating the multiple scenarios and facilitate a collaborative, multi-disciplinary approach to selecting the model to use for a baseline.
- How will our competitors and traditional referral partners recover?
- Assess the recovery timeline of key competitors in the market. If their ORs are not returning online soon, can we identify doctors and patients who would like to move ahead with procedures at our facilities?
- Reach out to key referral partners to understand their own recovery timeline. Will their extended closures or modified operations impact our pipeline?
- How will patients feel about coming back?
- Contact all patients with cancelled or delayed procedures, assure them of the safety and benefits of their treatment plan, and gauge their willingness to reschedule.
- In conjunction with normal scheduling confirmation policies, contact previously scheduled patients to assure them of the safety of keeping their appointments, and assess whether they still plan to proceed.
- What precautions are we going to take ensure the safety of our team members and patients? How will we promote those precautions to assure patients our facility is safe? How will we implement policies to ensure those precautions are effective?
Develop a Patient Prioritization Methodology
Once the potential demand for elective surgeries is understood, a health system must develop a prioritization process. This will ensure that the system can best serve its patient population by meeting the needs of the backlogged patients, current patients on the schedule as well as reserving some capacity for incoming new patients. Determining the appropriate methodology for your system will require a stakeholder group consisting of representatives from each clinical area. Additional support to provide supplemental, real-time analysis will enable rapid decision making.
There are several existing patient triage methodologies currently in place, including the overarching theme of saving “lives, organs, and limbs”. We have identified a few other unique perspectives for our clients to consider when developing their own prioritization methodology:
- From the patient’s perspective, what factors impact the prioritization process?
- What surgeries pose the greatest patient quality of life and safety risks due to delayed care?
- Will patients seek out new providers if they cannot receive treatment in a timely manner at their current provider?
- From the health system’s perspective, what factors impact the prioritization process?
- Should new patient acquisition be prioritized over retaining existing patients?
- How will the ever-changing market conditions be revisited to ensure our process stays updated?
- Analyze the financial impact of each surgery type. Can surgeries with the highest contribution margins be accelerated to relieve the system’s financial pressures?
- Are there any supply chain issues that may prohibit particular surgeries from occurring as soon as we would like them to?
- Which surgeries can be completed quickly and efficiently? Can we strike a balance between surgeries that require extensive post-operative care and those that do not?
- From the physician’s perspective, what factors impact the prioritization process?
- Which clinical area has the greatest backlog of demand? Will physician loyalty be impacted if we deprioritize certain service lines?
- Can we further optimize our schedule by grouping different case types together as they require the same physician, similar care teams, or similar OR prep?
Review Capacity Expansion Capabilities
As organizations start to prioritize cases, they must also be mindful of capacity constraints that may impact the ability to meet demand – key factors include staffing, medical supplies, and physical bed and OR capacity. In addition, hospitals should be mindful of reserving capacity for COVID-19 patients and any operational modifications that will decrease normal efficiency levels [e.g. patient testing]. Below are a few considerations to help systems understand their capacity constraints and resource needs:
- Can we extend the hours of our facilities?
- Can we expand the hours of the OR each day [into the evening]? Shift more elective surgeries to the weekends?
- Do we have the staff to accommodate these expanded hours? Are they willing and able to increase their hours? Have staff been impacted by furloughs/lay-offs?
- Can we expand our footprint?
- Are there surgeries that can be shifted to the outpatient setting?
- Can we partner with any local ASCs or other community providers to optimize access to facilities?
- Can telehealth be leveraged for pre- and post-op visits to expedite the perioperative process?
- What other operational constraints should we consider?
- How can our OR block schedule be optimized to drive efficiencies?
- How many of our ORs should be reserved for COVID-19 patients? Can we limit extended OR turnaround times to just COVID-19 reserved ORs?
- Can we support our capacity plans with the necessary surgical support services [Path/Lab, imaging, respiratory therapy, etc.]?
- What capacity should we reserve for emergent cases?
- What mechanisms can we put in place in case we need to throttle back surgeries in case of a COVID resurgence?
- What supplies and resources do we need to address COVID-19 patient testing prior to surgery? What supplies do we need for protecting staff during surgery?
Example Output
Below is a sample output of a client’s preliminary prioritization methodology. After quantifying demand, they discussed how each cohort of the demand [back-log patients, scheduled patients, and newly acquired patients] should be prioritized and ultimately decided that scheduled patients would take precedence, followed by backlogged patients, and finally newly- acquired patients. When overlaid onto capacity constraints, they were able to develop a go-forward schedule. This process is illustrated in the below graphic:
The calendar portion of the illustration depicts the proportions of each patient cohort that the system expects to treat each month. Key takeaways by month are listed below:
- Month 1
- Unscheduled capacity [Grey area] is significant and reserved for emergent or COVID-19 cases
- Excess capacity exists as patients are hesitant to immediately return to the hospital
- Equal amounts of capacity are dedicated to scheduled patients [Orange area] and back-log patients [Green area]
- Month 2
- Unscheduled capacity is reduced as patients become comfortable returning to the hospital; COVID-19 dedicated capacity decreases as the pandemic is contained
- Scheduled cases decrease as a result of a diminished pipeline during the peak of the crisis; capacity is shifted towards back-log patients
- Newly acquired patients [Blue] begin receiving treatment as strategies to alter historical referral patterns begin paying dividends
- Months 3 & 4
- Unscheduled capacity continues to erode as COVID-19 subsides and patients regain confidence in the health system
- Schedules begin to refill as operations recover
- The backlog is continuously reduced, allowing capacity to shift towards treating newly acquired patients
Conclusion
While your organization may not be past the peak impact of COVID-19, we encourage health systems to begin contemplating these issues now and to take the appropriate actions to prepare for their return to more normal healthcare services. We hope this approach helps your organization work through the complicated process of re-opening inpatient, elective procedures. If you have any comments or questions about this approach, please feel free to reach out to us here.
In the next part of this series, we discuss rebooting ambulatory services – read Part 2 here.
___
Note: Prior to re-opening, KCG encourages each health system to ensure they are following precautions that aim to prevent further transmission of COVID-19 outlined by CMS, the American Medical Association [AMA], and other medical professional organizations. Clearly set policies and agreement from stakeholders across the health system will be foundational to pursuing re-opening activities and will ensure that the health system is a safe zone for all.