Client Overview
The Gynecologic Oncology Program [Gyn/Onc] at the Medical University of South Carolina focuses on diagnosing and treating cancers of the pelvis & female reproductive systems. As one of the state’s only comprehensive Gyn/Onc programs, MUSC experiences consistently high volumes, with many patients traveling great distances for their care.
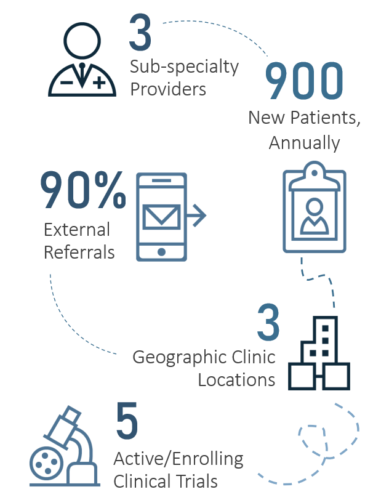
Due to the complexity of Gyn/Onc diagnoses & treatments, patients often require scans, labs, or consults from other sub-specialists to inform and advance care plans. Despite the need for an integrated approach to care, Gyn/Onc lacked the necessary infrastructure & processes to support this level of seamless care delivery, requiring patients to make multiple, often avoidable visits to MUSC.
The Solution
MUSC Health engaged KCG to assess Gyn/Onc’s seamless care performance. In this capacity, KCG conducted a thorough current-state assessment, identifying 20 large-scale initiatives and 80+ tactical recommendations for improvement. Then, partnering with Gyn/Onc leadership, KCG prioritized initiatives for implementation using a data-driven approach that delineated ‘low-hanging fruit’ from ‘longer-term strategic projects.’ Lastly, KCG worked with co-chairs and cross-departmental workgroups to drive the operationalization of each initiative. The findings of this assessment and opportunities for improvement identified fell into the following categories:
1. STAFFING MODEL: The Gyn/Onc clinic was supported by a matrixed staffing model comprised of operational, administrative, and clinical staff. However, due to misaligned reporting structures, roles were often unclear or subject to change on any given day. Early Wins: Developed an accountability matrix to clearly define staff roles and responsibilities, resulting in an initial cost savings of $140,000
2. TECHNOLOGY & TOOLS: The Gyn/Onc program did not effectively utilize the capabilities of its Epic or CareLink platforms to communicate or coordinate care across sites, process referrals, or drive efficient record collection from out-of-network providers. Early Wins: Implemented full suite of Epic tools and centralized referrals, streamlining administrative processes and enhancing outreach strategy.

3. CLINIC WORKFLOWS: Despite working with the same clinic staff, each physician had his/her own preferences & clinical protocols. These nuances led to role confusion, duplicative work, and lapses in standardization that resulted in an inconsistent patient experience. Early Wins: Adopted perioperative ERAS protocols and standardized physician templates, streamlining visit length and increasing patient access by 15%
4. CARE COORDINATION: Not all Gyn/Onc patients received the same level of perioperative patient education or care coordination, and the Nurse Navigator did not have sufficient bandwidth or supportive resources to coordinate care for all patients. Early Wins: Established a dedicated Gyn/Onc pre-op clinic and enriched education resources to ensure that all patients receive coordinated care
5. PHYSICIAN ENGAGEMENT: A significant disconnect between and among physicians and clinic staff created a culture of employee disengagement and prevented providers from collaborating, sharing best practices, or jointly pursue programmatic improvements. Early Wins: Increased alignment by implementing an inclusive monthly forum for physicians & clinic staff to discuss issues and identify solutions