Over the past few weeks, we’ve seen [and experienced] business operations across industries impacted by COVID-19 and the associated social distancing / shelter at home protocols. For healthcare providers, however, COVID-19 presents unique, more complex operational and financial challenges: unable to close their doors and ‘ride this out,’ healthcare providers are overwhelmed by the additional volume of COVID-19 cases. At the same time, they are still expected to provide care for those non- COVID-19 patients, many of whom are elderly and highly susceptible to the virus.
In response to this pressure, and as an attempt to stop the spread of coronavirus, the Trump Administration announced expanded telehealth benefits for Medicare beneficiaries during the COVID-19 outbreak. This action is intended to alleviate capacity pressures on healthcare facilities and personnel, as well as enable greater access to healthcare services without having to travel to a physical site.
Given that this a drastic departure from current telehealth policies, we’ve summarized the changes below and attempted to predict the long-term impact this may have on the healthcare industry.
Historical Background
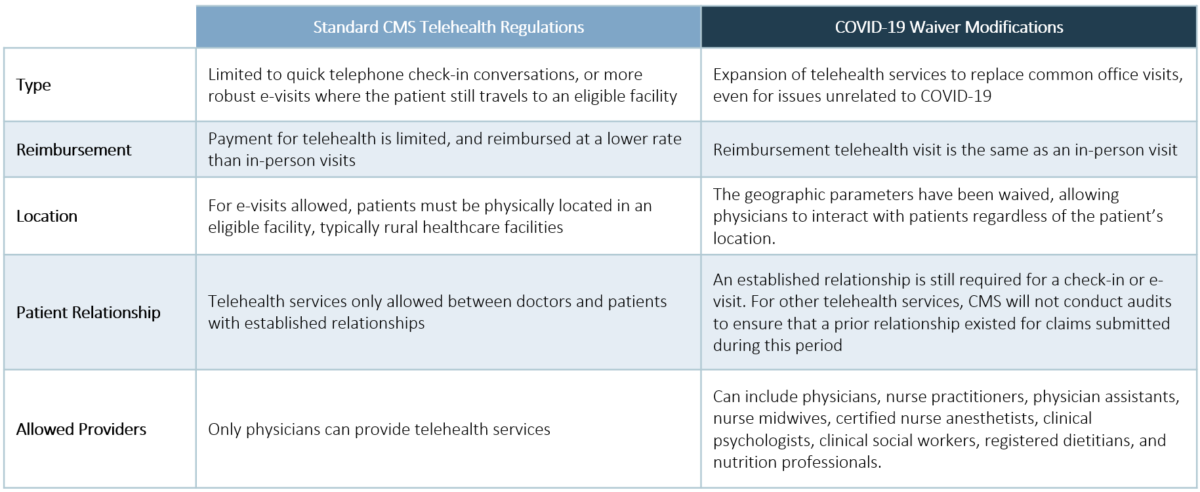
Historically, CMS has limited telehealth services for Medicare beneficiaries. Specifically, CMS had previously allowed quick [5 – 10 minutes] telephone conversations to take place between doctor and patient that may prevent an in-person follow-up visit. An additional regulation required that these visits take place between established doctor-patient relationships. These virtual check-ins, which are reimbursed at a lower rate than traditional visits, present a perverse incentive for providers.
Through another mechanism, CMS also allowed for more robust telehealth services termed “e-visits,” but only if the patient were in originating from eligible facilities. This generally meant the patient was physically located in a rural healthcare facility when the telehealth visit was initiated.
Enter Waiver 1135B
On March 6, 2020, President Trump signed H.R. 6074: Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. In addition to providing funding for vaccine development, it modified Section 1135(b) of the Social Security Act [Authority to Waive Requirements During National Emergencies] to enable providers to receive reimbursement for virtually interacting with Medicare beneficiaries during a Public Health Emergency, which we are experiencing now. The geographic parameters were waived, allowing physicians to interact with patients regardless of the patient’s location.
Additionally, these new telehealth visits are not restricted to COVID-19 related visits. For example, a Medicare beneficiary who is having issues managing their diabetes can interact with their doctor through a virtual platform, rather than meeting with them in person. Reimbursement for this type of telehealth visit is the same as an in-person visit, removing the perverse incentive.
In addition to the convenience of telehealth visits [many of us are aware that parking situations on healthcare campuses are far from ideal], it prevents our highest-risk patients from being exposed to COVID-19 and other contagions in a healthcare setting. The telehealth visits also allow for new patient-doctor interactions, which may be critical as many of our providers are at risk to contract COVID-19 and may not be available for patient visits.
What will this mean for the long-term?
Unfortunately, this solution may only be temporary as it is tied to the current healthcare crisis – however, we are hopeful that this waiver will serve as an effective ‘pilot’ and provide key insights to implementing a more robust and permanent solution. The government would also be wise to consult commercial payors who have expanded their policies to include telehealth visits in recent years [as a side note, some commercial payors have waived co-pays for telehealth services during the COVID-19 crisis]. We also believe that permanently expanding coverage could be a bipartisan effort as telehealth expands access to care, can be accomplished at a lower cost, and is supported by employers as it reduces the amount of time employees miss working hours to visit their doctors.
As we move through the crisis and return to normal operations, we envision that many healthcare systems will rethink their telehealth strategies – especially if a more permanent solution becomes available. If that’s the case, how will your organization leverage telehealth to provide more convenient care to patients? How much will be dependent upon reimbursement from CMS and commercial payors? Which strategies are dependent on patient population cohorts or are entirely agnostic to external factors?